Introduction to Diagnostic Medical Parasitology
Leishmaniasis, cutaneous
Essentials
Leishmaniae are protozoa belonging to the family Trypanosomatidae. On clinical grounds, they have been divided into three major groups: cutaneous, mucocutaneous and visceral. They consist of many different species and subspecies. Old World cutaneous leishmaniasis is due mainly to L. major, L. tropica and L. aethiopica. Leishmaniae are obligate intracellular parasites in host macrophages. They are transmitted to the mammalian host by bites of infected sandflies. Most species have an animal reservoir.
The female vector takes up blood with intracellular amastigotes which undergo morphogenesis in the insect gut and become promastigote forms with a flagellum. After regurgitation of promastigotes during a blood meal of the vector, promastigotes are taken up by host macrophages in which the promastigotes transform to amastigotes and start multiplying.
Epidemiology
- The geographical distribution of cutaneous leishmaniasis is species dependent:
L. major: India, central Asia, Middle East and parts of Africa
L. tropica: south-west Asia, Middle East and Mediterranean
L. aethiopica: Ethiopia and Kenya - Prevalence is correlated with the exposure to Phlebotomus spp. vectors
- All cutaneous Leishmania species (except L. tropica) have an animal reservoir (zoonosis)
Pathology
- Localized, self-limiting skin ulcer (“Oriental sore”) elicited by multiplying amastigotes (healing after several months)
- Diffuse cutaneous leishmaniasis: chronic infection with multiple lesions
Clinical Findings
- Incubation period at least 1 week up to many months!
- The disease starts with a papula which enlarges and typically becomes an indolent ulcer
- Bacterial infection of the ulcer is common
- Lesions may heal spontaneously within weeks or months, or may persist for a year or more

Diagnosis
Diagnostic methods
Parasitological diagnosis
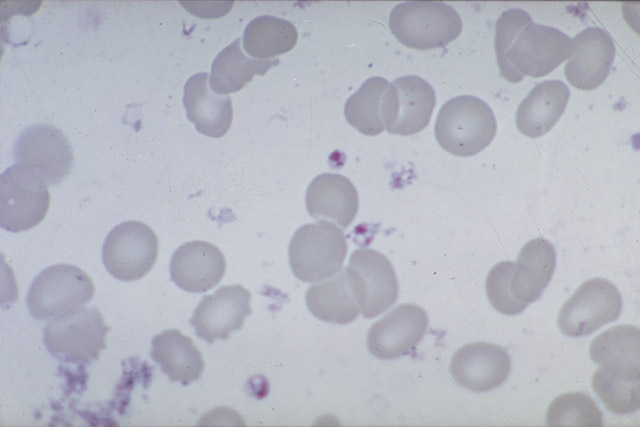
Direct microscopy of skin biopsies (stained sections or smears) detecting amastigotes has a low sensitivity (50–70%). Somewhat better results – but with a delay – are obtained after cultivation. However, these traditional methods have now been replaced by molecular diagnostic tests.
Molecular diagnosis
Early DNA hybridization methods with specific probes have now been replaced by various PCR methods which are reaching “gold standard” status. In contrast to microscopy, molecular methods can distinguish species and subspecies of Leishmania by RFLP analysis of the amplicon.
Antigen detection
No tests developed
Antibody detection
No circulating antibodies can be detected in most cases of cutaneous leishmaniasis
Diagnostic strategies
The diagnosis relies mainly on clinical findings. Today an optimal diagnostic strategy uses molecular diagnostic methods.
Prevention and control
- Individual protection by fine-mesh fly netting and residual spraying
- Eliminate breeding places of sandflies
- Elimination of reservoir animals near habitations