Introduction to Diagnostic Medical Parasitology
Amoebiasis
Essentials
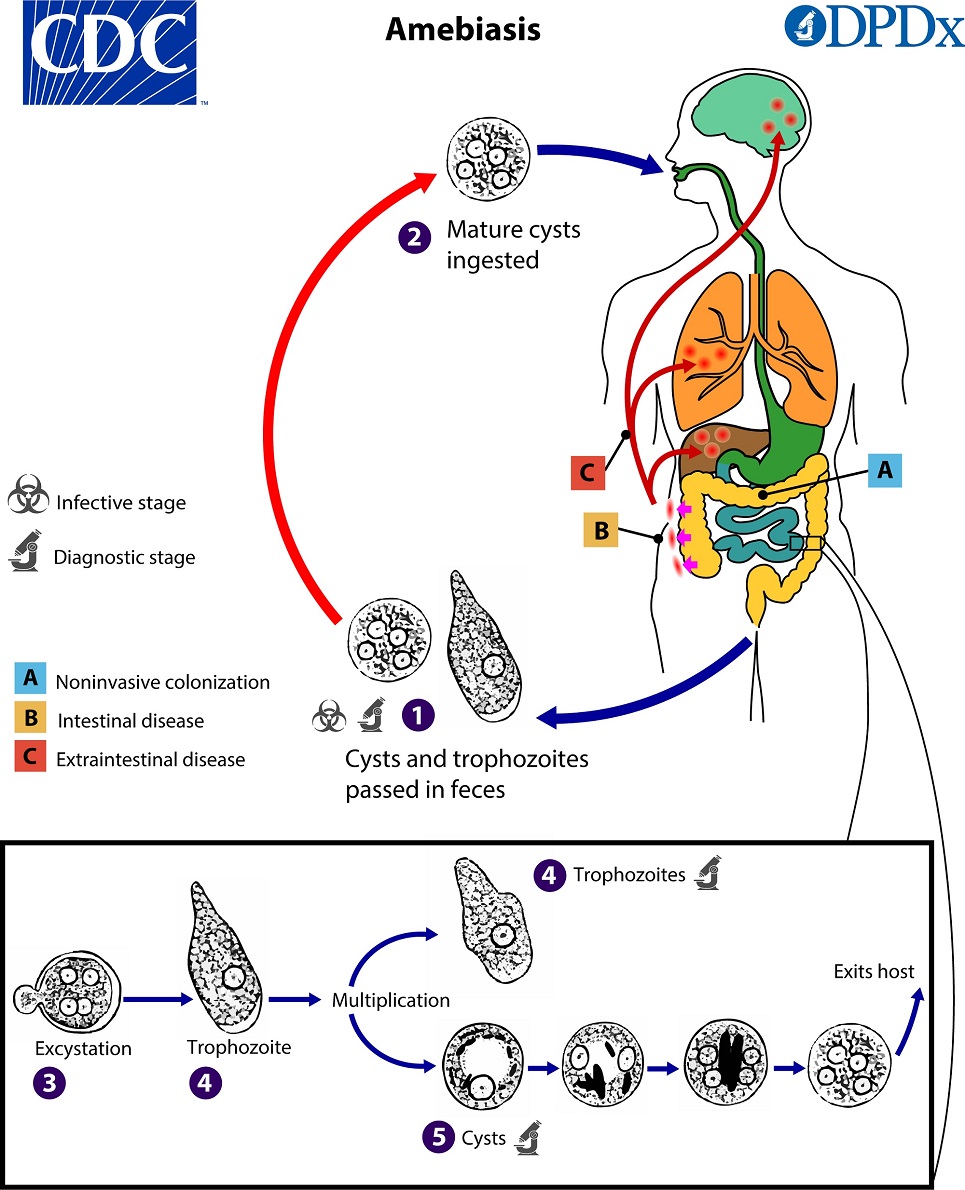
Entamoeba histolytica, a potentially pathogenic amoeba of humans, lives as trophozoites in the intestine and produces cysts which are passed in faeces and which assure faecal-oral transmission. This parasite may invade tissues and give rise to intestinal or extra-intestinal diseases (amoebic dysentery or amoebic abscesses). The morphological differentiation of amoebae as cysts or trophozoites needs good microscopic skills. The non-pathogenic E. dispar is morphologically identical to E. histolytica. It can only be differentiated by molecular methods.
Epidemiology
- Worldwide distribution, but prevalence higher in tropical areas!
- Susceptibility: children are particularly susceptible, but the disease is less common in those under 5 years. Liver abscesses are found predominantly in males.
- The main transmission mode is by ingestion of cysts with faecally contaminated food or water. The cysts survive for weeks or months in the soil (if temperature is not below 4 or above 40 °C). They are chlorine resistant!
- Asymptomatic cyst passers are important for spreading the disease!
Pathology
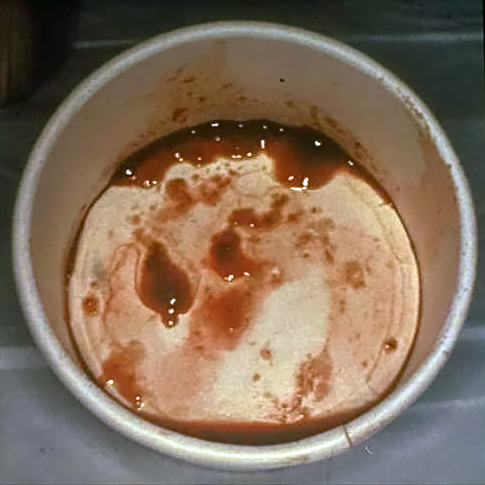
- Invasion of large-bowel mucosa leads to ulceration and often bloody diarrhoea
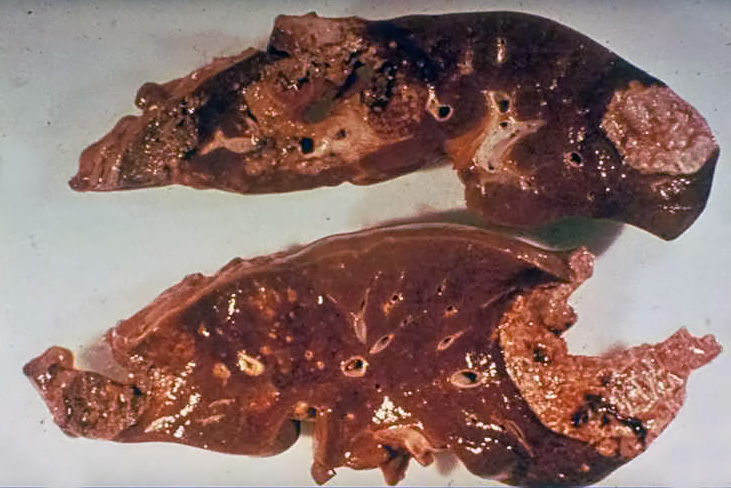
- Extra-intestinal invasion causes mainly liver abscesses, and occasionally abscesses of the lung or brain
- E. histolytica produces cytopathogenic effects on mammalian cells by “toxins”
Clinical Findings
Clinical findings vary considerably. The main findings are:
- Asymptomatic amoebiasis (healthy cyst passers)
- Chronic amoebiasis with diarrhoea, and sometimes mucus
- Acute amoebiasis with dysentery and fever
More rarely: amoebic granulomata (in the wall of the large intestine) – often misdiagnosed as carcinoma – and ulceration in the perianal region
- Extra-intestinal amoebiasis: dissemination in the bloodstream produces liver abscesses, and occasionally abscesses of the lung and brain.
Diagnosis
Diagnostic methods
Parasitological diagnosis
In a case of amoebic dysentery, diagnosis is by microscopic identification of trophozoites or cysts in fresh faecal specimens. A well-trained microscopist is needed because E. histolytica must be differentiated from non-pathogenic amoebae and macrophages. Microscopically the pathogenic amoeba E. histolytica cannot be distinguished from non-pathogenic E. dispar (unless amoebae contain phagocytosed erythrocytes: only E. histolytica is haematophagous!).
In extra-intestinal amoebiasis (suspicion of an amoebic liver abscess), aspirates of abscesses can be investigated.
Molecular diagnosis
The Gastro-acute Panel is used for the rapid investigation (within a maximum of 2 hours after sample arrival) of acute diarrheal diseases. It includes bacteria and viruses, as well as the most common protozoa. In cases of mixed infections, assessments regarding the dominant pathogen can be made after a telephone consultation.
The Protozoa Panel is used to investigate chronic gastrointestinal complaints and covers the main pathogenic agents, as well as additional facultative pathogenic pathogens. All pathogens can also be requested as individual tests.
Individual tests for protozoa involve the identification of pathogens by detecting their DNA or RNA.
Serological detection
Method: ELISA, IFAT
Note: Uncertain titers should be rechecked after 1 week. Post-therapy, a significant increase in titer is observed within a few days. A noticeable decline in a positive titer is typically detectable around 6 months after therapy. Serology is almost always negative in non-invasive intestinal amoebiasis. In cases of a liver abscess, intestinal infections are usually no longer microscopically detectable. For detecting amoebas in aspirates, PCR is significantly more promising than microscopic examination.
Diagnostic strategies
- To diagnose a suspicious case of invasive amoebiasis
For screening, serology is the first choice. In early infection, serology might be negative due to the retarded detection of circulating antibodies. Amoebae can also be detected in abscess aspirates by microscopy or PCR. Stool examinations are often negative in invasive amoebiasis.
- To detect asymptomatic carriers of E. histolytica
Screen stool samples with an antigen detection assay or with PCR. Microscopy and serology have no diagnostic value for carriers!
Prevention and control
Education in public hygiene
- Protection of the public from faecal contamination
- Sanitary disposal of human faeces
- Training in thorough hand washing after defecation
Protection of water supplies from faecal contamination
- Problems with surface water
- Sedimentation and filtration of water is preventive but chlorination is not
